Healthcare provides services, and this process makes sure they get money from patients’ insurance. Knowing this process is a big deal for doctors, the insurance companies, and patients. About the medical billing steps and how to make it better. We will explain each step and what’s important for getting paid right and on time.
The medical billing process is a crucial component of healthcare industry, ensuring that the healthcare providers receive compensation for the care and services they provide. In this guide, what is the process of medical billing, outline each step involved, discuss strategies to improve the medical billing process, procedures for maximum efficiency and accuracy.
What is the Process of Medical Billing?
The process of medical billing translates the medical services into standardized billing claims to ensure the healthcare providers receive compensation. Medical billing is essential for the financial health of clinics, hospitals, and the practices as it manages the financial exchanges between patients, healthcare providers and insurers. The medical billing process starts when a patient schedules an appointment, continues through verification, coding, claim submission and the final payment processing.
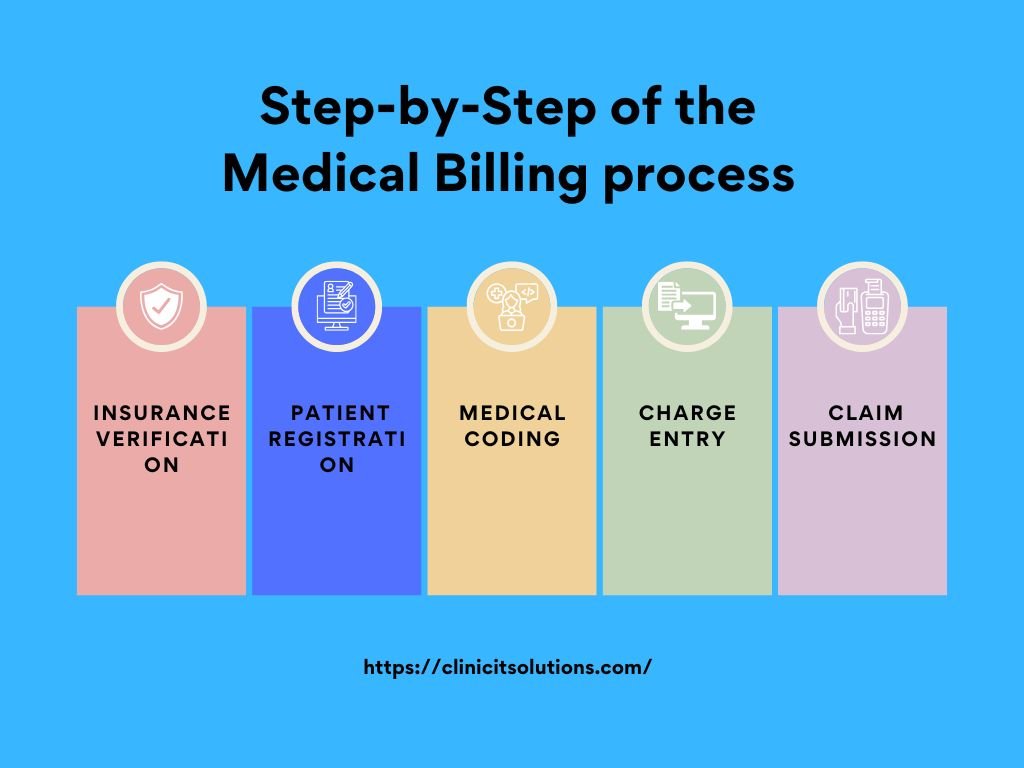
Insurance Verification
Once you collected the patient’s information proceed with insurance verification. The patient’s insurance company to validate the eligibility and coverage specifics. For this process, we will determine whether the patient’s insurance policy is active and if it includes the services being offered.
Patient Registration
The process of the medical billing starts with registration of patient. The essential information that is gathered includes.
Patient’s information (name, address, date of birth)
Insurance details (primary and secondary insurance providers)
Purpose of the visit
Referring doctor (if applicable)
Medical Coding
One of the most complex stages in the medical billing procedure is medical coding. In this step, standardized codes (like CPT, ICD-10, and HCPCS) are allocated to the services rendered. The errors in coding can result in claim denials or postponed payments. The primary coding systems utilized by coders are:
- ICD (International Classification of Diseases) codes for diagnoses
- CPT (Current Procedural Terminologies) codes for procedures
Charge Entry
Once the medical services have been coded and the next step in the medical billing process is charge entry. The procedures are technically coded, the biller receives codes and the charges for services provided by the practitioner to create a claim for reimbursement.
- Codes are aligned with the correct fees
- Relevant modifiers are applied
- The total charges for the encounter are calculated
Claim Submission
After charge entry the medical billing process moves to claim submission. This stage includes the development of an electronic or paper claim form that includes:
- Patient details
- Insurance details
- Diagnosis codes
- Procedure codes
- Fees for services provided
Payment Posting
Upon receiving payments from insurance payers, the next step is payment posting and the insurance company will send a payment remittance advice to your practice.
This document contains details of the payment made by insurance company for the services you rendered. During the payment posting, your staff will record and post this payment to the patient’s account. The posting reflects the amount paid by insurance company and any remaining balance that needs to be addressed to the patient later.
Denial Management
Not every claim gets approved upon the initial submission. Denials can occur for various reasons, such as errors in coding or a lack of pre-authorization. They consist of recognizing and resolving the causes of claim denials, resubmitting corrected claims, and appealing when necessary. It is essential for recovering payments that would otherwise be lost.
A/R Follow-up
A/R follow-up refers to Accounts Receivable follow-up. It’s the process where businesses track and manage payments owed by customers.
This involves contacting customers who haven’t paid their invoices on time, sending reminders, or negotiating payment terms to ensure the business receives the money it’s owed. Ensures a smooth financial interaction between healthcare provider and the patient.
Reporting and Analysis
The final step in medical billing process is reporting and analysis. This involves generating reports to:
- Track key performance indicators (KPIs)
- Identify trends in claim denials or payments
- Analyze the overall financial health of the practice